Non-Pharmacological Interventions for Dementia
Approximately 1.6 million people with dementia are living in Germany now.
These people as well as their relatives are facing the challenge of mastering everyday life and keeping on enjoying life despite of limited cognitive performance due to dementia. The possibilities of pharmacological treatment for dementia are very limited.
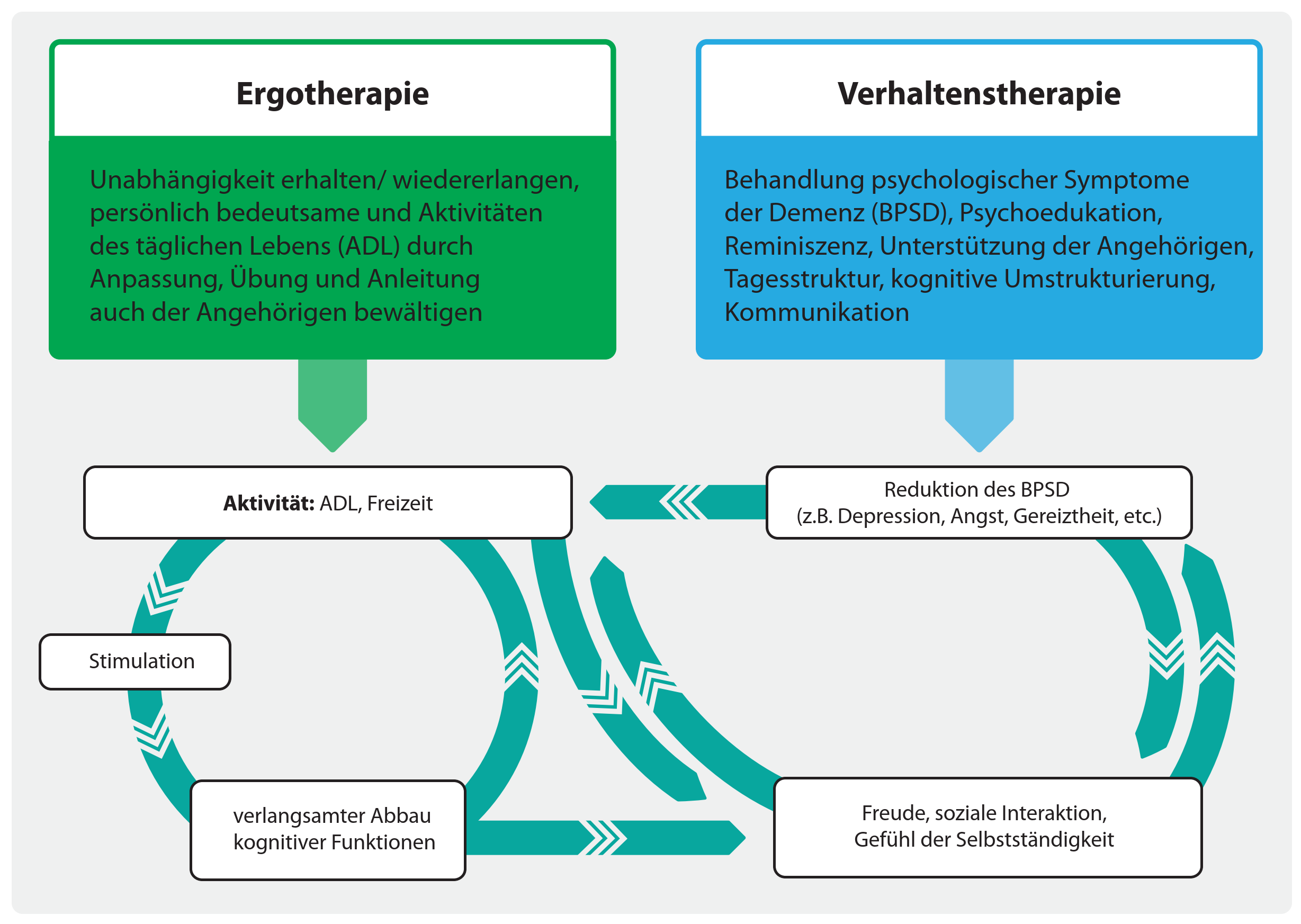
Non-pharmacological interventions offer valuable support.
This website mainly informs about occupational and behavioural therapy for people with dementia and their family caregivers because these interventions have shown to be effective particularly close to everyday life.1
Of course, there are additional non-pharmacological interventions for dementia, such as cognitive stimulation, logopaedics, physiotherapy, milieu therapy, music therapy etc.


Quelle: Deutscher Verband der Ergotherapeuten DVE (German Association of occupational therapists) - https://dve.info/service/presse/pressefotos
Occupational Therapy for people with dementia and their family caregivers
Occupational therapy is a structured treatment that aims at sustaining as much independence as possible in the personally relevant areas of life and interests of people with dementia. The living environment is being particularly considered, and the involvement of relatives is intended.
Occupational Therapy for Dementia - A Brief Overview
Occupational Therapy is way more than occupation.
Occupational Therapy for people with dementia provides support for personally relevant daily activities and thus contributes significantly to sustaining independence and satisfaction of people with dementia, as well as to lessen the burden for family caregivers.The therapy contains (among other things):
- daily activities - individual priorities, interests and strengths are considered
- counselling/education for family caregivers – regarding the course of the disease, ADL training, resources etc.
- (re)arrangement of the environment – to reduce falls, to strengthen orientation etc.
- practice of the use of aids – e.g., training to use a walker-rollator
Occupational Therapy has a positive impact in the following areas:
- independence of people with dementia is increased and/or sustained 1, 2
- people with dementia are being mobilized and can (again) pursue their important activities, 1, 3 which increases their self-esteem
- problematic behaviour is reduced 1, 4
- quality of life is increased 4
- strain for family caregivers is reduced 2, 4
The supply of Occupational Therapy can be extrabudgetary for dementia.
Occupational Therapy should take place as a home visit, as the personal living environment is constantly being referred to.
Occupational Therapy can be applied in different stages but should ideally be initiated when the diagnosis is made.
The “S3-Leitlinie Demenzen” (S3 guidelines for dementia) recommends ADL training for dementia.
“There’s evidence that occupational, individually tailored interventions for patients with mild to moderate dementia with the involvement of reference persons contributes to sustaining daily function. The application should be offered.”Empfehlungsgrad B, Evidenzebene Ib, Leitlinienadaptation NICE-SCIE 2007 (S3-Leitlinie Demenzen der Deutschen Gesellschaft für Neurologie, & Deutschen Gesellschaft für Psychiatrie und Psychotherapie, Psychosomatik und Nervenheilkunde)
A few evidences of efficacy
[1] Gitlin, L., Corcoran, M., & Winter, L. (2001). A randomized, controlled trial of a home environmental intervention: Effect on efficacy and upset in caregivers and on daily function of persons with dementia. The Gerontologist, 41, 4-14. https://doi.org/10.1093/geront/41.1.4
[2] Graff, M. J. L., Vernooij-Dassen, M. J. M., Thijssen, M., Dekker, J., Hoefnagels, W. H. L., & Olde Rikkert, M. G. M. (2006). Community based occupational therapy for patients with dementia and their care givers: randomised controlled trial. BMJ, 333, 1196-1199. https://doi.org/10.1136/bmj.39001.688843.BE
[3] Phinney, A., Chaudhury, H., & O’Connor, D. L. (2007). Doing as much as I can do: The meaning of activity for people with dementia. Aging & Mental Health, 11, 384-393. https://doi.org/10.1080/13607860601086470
[4] Pimouguet, C., Le Goff, M., Wittwer, J., Dartigues, J.-F., & Helmer, C. (2016). Benefits of occupational therapy in dementia patients: Findings from a real-world observational study. Journal of Alzheimer’s Disease, 56, 509-517. https://doi.org/10.3233/JAD-160820
Bibliography
Flotho, W., & Sibold, C. (2014). HED-I Häusliche Ergotherapie bei Demenz. Interventionsprogramm für Menschen mit leichter bis mittlerer Demenz und ihre Angehörigen im häuslichen Umfeld. Idstein: Schulz-Kirchner.
Gitlin, L., & Corcoran, M. (2005). Occupational therapy and dementia care. The home environmental skill-building program for individuals and families. North Bethesda, MD: American Occupational Therapy Association, Inc.
Holthoff, V., Reuster, T., & Schützwohl, M. (2013). ERGODEM. Häusliche Ergotherapie bei Demenz - ein Leitfaden für die Praxis. Stuttgart: Thieme.
Voigt-Radloff, S., Rühlemann, A., & Hüll, M. (2012). WHEDA - Wirksame Häusliche Ergotherapie für Demenzerkrankte und Angehörige. Behandlungsmanual. Idstein: Schulz-Kirchner.
Further information can be found at:
DVE (Deutscher Verband der Ergotherapeuten / German Association of Occupational Therapists):
BED (Bundesverband für Ergotherapeuten in Deutschland e.V. / Federal Association for Occupational Therapists in Germany e.V.):
Frau Gudrun Schaade (Occupational therapist, author):
[1] Frankenstein, L. & Jahn, G. (2020). Behavioral and Occupational Therapy for Dementia Patients and Caregivers. GeroPsych, 33. https://econtent.hogrefe.com/doi/abs/10.1024/1662-9647/a000225
Behavioural Therapy for people with dementia and their family caregivers
With the help of behavioural therapy, psychological symptoms of dementia, such as depression, anxiety, apathy, or agitation can be reduced. Conflicts can be prevented and everyday life of people with dementia can be structured in a meaningful way.
Behavioural Therapy for Dementia – A Brief Overview
Behavioural Therapy can also be of great use for people with dementia.
Behavioural Therapy can help people with dementia to accept the diagnosis, prepare them for everyday life with limited cognitive capacity and reduce secondary symptoms like depression or anxiety.
It helps family caregivers to better understand the person with dementia, avoid conflict, and increase a feeling of competence. Thus, depressive symptoms can be obviated.
The therapy consists of (among other things):
- structuring the day to increase and stabilize daily activities
- biographical work to conserve cognitive functioning and strengthen a sense of self-esteem
- behavioural management to reduce challenging behaviour
- couple counselling and communication training to dissolve conflicts caused by dementia
- changing dysfunctional cognitions for a new assessment of living conditions
Behavioural Therapy has a particularly positive impact on the following areas:
For people with dementia- secondary symptoms like depression, anxiety 1, 6
- quality of life and well-being 5, 7
- activity and activities of daily living 5
- cognitive performance 5, 7, e.g., attention, concentration, memory
For relatives of people with dementia
- depressive symptoms 3, 8
- quality of life 4
- stress 3, 8 and burden 1, 4
- sense of competence4
The S3-Leitlinie Demenzen (S3 guideline for dementia) recommends psychosocial interventions, such as reminiscence therapy and training for relatives.2
Prescription
Behavioural Therapy is especially suited for people with mild to moderate dementia and their family caregivers. If possible , the intervention should be initiated, when the diagnosis is made.
Health insurances usually only cover the costs of Behavioural Therapy if the person with dementia additionally has secondary symptoms (e.g., depression, anxiety) or if the family caregiver develops an adjustment disorder.
A few evidences of efficacy
[1] Baharudin, A., Che Din, N., Subramaniam, P., & Razali, R. (2019). The associations between behavioral-psychological symptoms of dementia (BPSD) and coping strategy, burden of care and personality style among low-income caregivers of patients with dementia. BMC Public Health, 19. https://doi.org/10.1186/s12889-019-6868-0
[2] Deutsche Gesellschaft für Neurologie, & Deutsche Gesellschaft für Psychiatrie und Psychotherapie, Psychosomatik und Nervenheilkunde (2016). S3-Leitlinie Demenzen. Stand: 24. Januar 2016. DGPPN & DGN. https://www.awmf.org/uploads/tx_szleitlinien/038-013l_S3-Demenzen-2016-07.pdf
[3] Hopkinson, M. D., Reavell, J., Lane, D. A., & Mallikarjun, P. (2018). Cognitive behavioral therapy for depression, anxiety, and stress in caregivers of dementia patients: A systematic review and meta-analysis. The Gerontologist, 59. https://doi.org/10.1093/geront/gnx217
[4] Jütten, L. H., Mark, R. E., Wicherts, J. M., & Sitskoorn, M. M. (2018). The Effectiveness of psychosocial and behavioral interventions for informal dementia caregivers: Meta-analyses and meta-regressions. Journal of Alzheimer’s Disease, 66. https://doi.org/10.3233/JAD-180508
[5] McDermott, O., Charlesworth, G., Hogervorst, E., Stoner, C., Moniz-Cook, E., Spector, A., Csipke, E., Orrell, M. (2019). Psychosocial interventions for people with dementia: A synthesis of systematic reviews. Aging & Mental Health, 23. https://doi.org/10.1080/13607863.2017.1423031
[6] Orgeta, V., Qazi, A., Spector, A., & Orrell, M. (2015). Psychological treatments for depression and anxiety in dementia and mild cognitive impairment: systematic review and meta-analysis. The British Journal of Psychiatry, 207. https://doi.org/10.1192/bjp.bp.114.148130
[7] Pinquart, M., & Forstmeier, S. (2012). Effects of reminiscence interventions on psychosocial outcomes: A meta-analysis. Aging & Mental Health, 16. https://doi.org/10.1080/13607863.2011.651434
[8] Selwood, A., Johnston, K., Katona, C., Lyketsos, C., & Livingston, G. (2007). Systematic review of the effect of psychological interventions on family caregivers of people with dementia. Journal of Affective Disorders, 101. https://doi.org/10.1016/j.jad.2006.10.025
Bibliography
Forstmeier, S., & Roth, T. (2018). Kognitive Verhaltenstherapie für Patienten mit leichter Alzheimer-Demenz und ihre Angehörigen. Springer.
Häusler, A., Krause-Köhler, K., Niemann-Mermehdi, M., Nordheim, J., & Rapp, M. (2014). Psychosoziale Therapie bei beginnender Demenz. Das Unterstützungsprogramm für Menschen mit Demenz und ihre Partner. Mabuse-Verlag.
Werheid, K., & Thöne-Otto, A. (2010). Alzheimer-Krankheit. Ein neuropsychologisch-verhaltenstherapeutisches Manual. Beltz.
Further information can be found at:
Deutsche Alzheimer Gesellschaft (German Alzheimer‘s Association):
Papers about non-pharmacological interventions for dementia:
https://www.doctors.today/a/nichtmedikamentoese-therapie-der-demenz-mit-ergotherapie-alltagskompetenz-erhalten-2307724
https://www.landesinitiative-demenz.de/aktuelles/neuigkeiten/ergotherapie-und-verhaltenstherapie-bei-demenz-hausaerztinnen-informieren
Further Information about non-pharmacological interventions for dementia:
Straubmeier, M., Behrndt, E.-M., Seidl, H., Özbe, D., Luttenberger, K., & Gräßel, E. (2017).
Non-pharmacological treatment in people with cognitive impairment. Deutsches Ärzteblatt International, 114.
https://doi.org/10.3238/arztebl.2017.0815
https://www.demenz-aktuell.de/therapie
If you have any questions or comments, feel free to contact me





